Blood Typing and Screening
Update October 29, 2018
Blood transfusions in humans were risky procedures until the discovery of the major human blood groups by Karl Landsteiner, an Austrian physician, in 1900.
Until that point, physicians did not understand that death sometimes followed blood transfusions, when the type of donor blood infused into the patient was incompatible with the patient’s own blood.
Blood groups are determined by the presence or absence of specific antigens on the plasma membranes of erythrocytes. With their discovery, it became possible for the first time to match patient-donor blood types and prevent transfusion reactions and deaths.1
More than 50 antigens have been identified on erythrocyte membranes, but the most significant in terms of their potential harm to patients are classified in two groups: the ABO blood group and the Rh blood group.
Reearch Frontier
Newly Found Enzymes Can Help Turn Type A and B Blood into Universal Type O1
http://www.sci-news.com/medicine/enzymes-turn-type-a-b-blood-into-universal-type-o-06324.html
++++++++++++++++++++++++++
The most important is the ABO Group.
In transfusion reactions, antibodies attach to antigens on the surfaces of erythrocytes and cause agglutination and hemolysis.
Hemolytic transfusion reactions (HTR) are systemic reactions provoked by immunologic red blood cell (RBC) incompatibility. Clinical and experimental observations of such reactions indicate that they proceed through phases of humoral immune reaction, activation of phagocytes, productions of cytokine mediators, and wide-ranging cellular responses. HTR have many features in common with the systemic inflammatory response syndrome (SIRS). Knowledge of the pathophysiologic mechanisms in HTR suggest that newer biological agents that target complement intermediates or proinflammatory cytokines may be effective agents in the treatment of severe HTRs.2
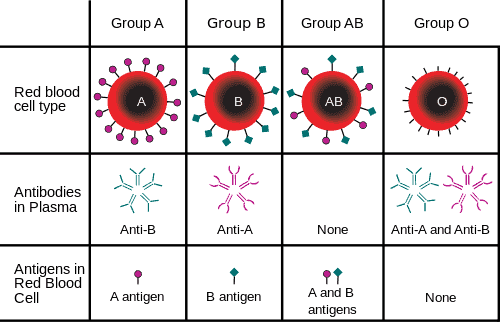
ABO blood group
ABO blood group antigens are designated A and B.
People with type A blood have A antigens on their erythrocytes, whereas those with type B blood have B antigens. Those with AB blood have both A and B antigens, and those with type O blood have neither A nor B antigens. The blood plasma contains preformed antibodies against the antigens not present on a person’s erythrocytes.
A second group of blood antigens is the Rh group, the most important of which is Rh D. People with Rh− blood do not have this antigen on their erythrocytes, whereas those who are Rh+ do. About 85 percent of Americans are Rh+. When a woman who is Rh− becomes pregnant with an Rh+ fetus, her body may begin to produce anti-Rh antibodies. If she subsequently becomes pregnant with a second Rh+ fetus and is not treated preventively with RhoGAM, the fetus will be at risk for an antigen-antibody reaction, including agglutination and hemolysis. This is known as hemolytic disease of the newborn.
Cross matching to determine blood type is necessary before transfusing blood, unless the patient is experiencing hemorrhage that is an immediate threat to life, in which case type O− blood may be transfused.
Before a transfusion is given, the donor blood must not contain antibodies against the antigens present in the red cell of the recipient.
This is accomplished by determining the blood type of the donor and the blood type of the recipient.
Blood from the Donor
Blood from the donor is first typed for the presence of A and B antigens as well as D antigen on the red cells.
The addition of serum containing a high titer of anti-A antibody (from a Type B donor) will result in prompt clumping (agglutination) of type A or AB red cells, whereas type O red cells remain in a uniform suspension.
In a like manner, this simple agglutination test is also used to determine whether red cells express B and D antigens.]
The blood of a patient who is to receive red cell transfusions undergoes the same ABO and D typing as described for donor units. In addition, the patient's serum is tested for the presence of alloantibodies other than anti-A and anti-B.
------------------------------------------------------------------------------------------------------------------------------------------------------------
Screening for Alloantibodies
Figure below shows an example of the use of red cells from two individuals carefully selected to differ not only in the Rh C, c, E, and e antigens but also in other antigen systems (Kell and Duffy). If the patient's serum fails to agglutinate cells from either of these donors, it lacks alloantibodies to these antigens. Note, however, that the patient's serum in fact agglutinates the red cells of donor 2. This result indicates that the patient has alloantibodies to E, c, or Fyb, or possibly a combination thereof, but no alloantibodies to D, C, e, K, k, or Fya.
The blood bank then uses additional panels of red cells to identify the patient's specific alloantibody or alloantibodies. This information allows the blood bank to select units that not only have the same ABO and D type as the patient but also lack the antigens to which the patient is immune. As a further safeguard, each selected donor unit is then tested against serum from the patient by means of the indirect antiglobulin test (indirect Coombs test, Figure) to ensure that the unit is fully compatible.
Use of two panels of antigenically characterized red cells to test a patient's serum for the presence of alloantibodies. The interpretation of the results shown is explained in the text.
